The impact of early detection and intervention on congenital heart defects in infants and children: a systematic review
Keywords:
Congenital heart defects, Early detection, Infants, ChildrenAbstract
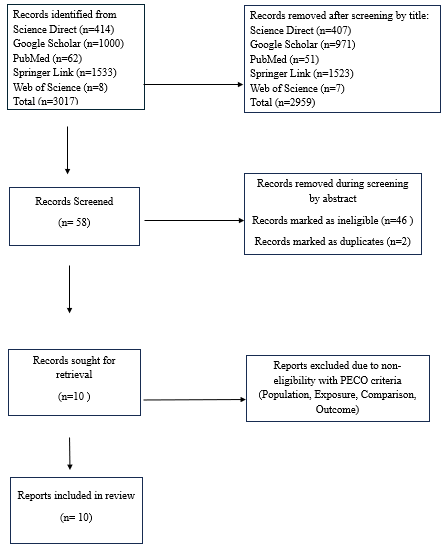
Congenital heart disease (CHD) is the leading cause of mortality among congenital disabilities, affecting approximately 1% of live births. This review analyzes the critical role of early detection and intervention strategies in optimizing care for pediatric patients with CHD, utilizing a comprehensive literature search across scientific databases such as Google Scholar, PubMed,Web of Science, Springer Link, and Science Direct for articles published between 2014 and 2024. A total of 10 studies were included, representing diverse populations and healthcare systems, which provided a global perspective on CHD prevalence and diagnosis in infants and children. These studies, comprising case-control studies from Mount Sinai Medical Center, cohort studies from regions such as Denmark, Paris, Saudi Arabia, and Australia, and cross-sectional studies from China and France/Belgium, highlight the clinical challenges associated with CHD and the long-term developmental and psycho-social implications for affected children. The findings underscore the necessity of continued efforts in maternal health, early screening, and holistic care approaches to improve outcomes for children with CHD worldwide. Ultimately, the review emphasizes that early detection is crucial for enhancing survival rates and quality of life and advocates for integrating medical and psycho-social support to address the multifaceted needs of these children.
Published
How to Cite
Issue
Section
Copyright (c) 2025 R. T. Akah, J. E. Enoh, B. Nkeh-Chungag

This work is licensed under a Creative Commons Attribution 4.0 International License.